YOUR PHYSIO
Condition directory
Thumb Osteoarthritis
 Osteoarthritis is the most common form of arthritis. Contrary to popular belief osteoarthritis is not caused by aging and does not necessarily deteriorate. Osteoarthritis can affect people in different ways – some people may only experience mild symptoms whereas others can experience more severe symptoms. Interestingly some patients can even have osteoarthritis and be completely pain free!
Osteoarthritis is the most common form of arthritis. Contrary to popular belief osteoarthritis is not caused by aging and does not necessarily deteriorate. Osteoarthritis can affect people in different ways – some people may only experience mild symptoms whereas others can experience more severe symptoms. Interestingly some patients can even have osteoarthritis and be completely pain free!
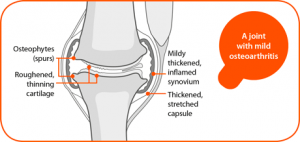
At the end of each bone we have a type of cartilage known as hyaline cartilage. Over our lifetime a variety of traumas may trigger this cartilage or a joint to repair itself. Your body attempts to lay down extra bone to repair the area. This is a very slow and efficient inflammatory process. Usually we are left with a structurally altered but pain free joint. However, if a trauma is too significant or the joint is unable to compensate then people may become symptomatic. If you break the word arthritis down, “arth” means bone and “it is” means inflammation. Often people will go through an inflammatory phase with can settle with good management and time. See below for further advice.
Osteoarthritis can effect may people in different ways. Interestingly, the severity does not always reflect There is a known poor correlation between changes visible on x-ray and symptoms of osteoarthritis – minimal changes may cause a severe amount of pain and severe changes may be symptom free.
Osteoarthritis may be suspected if you are over 45 years old, experience activity related joint pain and morning stiffness/stiffness related to inactivity. Further tests such as X-rays and blood tests are often not required although may be completed to rule out other possible causes of symptoms.
The symptoms associated with osteoarthritis usually are:
- Joint stiffness and pain (particularly if you haven’t moved the joint for a while)
- Limited range of movement of a joint
- Joint swelling
- Slightly thickened or enlarged appearance to the joint
- A grating sensation of a joint known as crepitus
There are certain factors which may lead you more prone to osteoarthritis – these include:
- Family history of osteoarthritis
- Repeated traumas or significant injury to a joint
- Gender – women are more likely to develop osteoarthritis
- Obesity
- Age – although this is not a normal part of aging, the risk of osteoarthritis increases with age – we all get grey hairs and wrinkles and the same changes occur internally
 Osteoarthritis can affect any part of the body but the most common areas are the weight baring joints of knees/hips and the small joints of the hands.
Osteoarthritis can affect any part of the body but the most common areas are the weight baring joints of knees/hips and the small joints of the hands.
The most common site of arthritis in the hand is at the base of the thumb (see diagram above). This occurs at a joint known as the carpo-metacarpal joint. This joint is a saddle joint which means that the surfaces are convex in one direction and concave in the other that allow the thumb to be very flexible and mobile.
If you were to develop osteoarthritis at this joint you may notice a reduction in range of movement of the thumb, increased pain with certain activities and weakness in grip strength. Maintaining your range of movement and strength will be beneficial in order to maintain good levels of function.
The current arthritis guidelines recommend the use of paracetamol and/or non-steroidal anti-inflammatories (NSAID’s) for the management of arthritic pain. Both types of medication are available over the counter at your local pharmacy. We would always advise discussing your suitability for the medication with the Pharmacist before starting a course of treatment.
Often people may report difficulties with specific tasks or activities that involve gripping. It may be helpful to modify or adapt how you complete these activities to make it more comfortable. Simply pacing or completing tasks to a tolerance level only can be helpful rather than pushing into pain. Where possible it may be helpful to purchase equipment or kitchen aids to help with difficult tasks.
If symptoms are becoming unmanageable, a night resting splint may be provided which can help to give the joint some relative rest to help symptoms settle. The most effective splint is thermoplastic and requires moulding to the individual. Your physiotherapist could supply and fit one if required. If you would like further physiotherapy advice for this condition, you can always be referred to our service.
Should symptoms fail to settle, an anti-inflammatory corticosteroid injection maybe helpful to ease symptom. Your GP or the MSK team may be able to perform the injection for you.